By Shadi Jurdi, MD
Senior Medical Director
Quantum Health
Every problem begins with a pain. With musculoskeletal (MSK) conditions, employers have three: cost, prevalence and the disconnect between the employees who are suffering and the MSK treatment and health benefits they need but don’t fully understand. Bridging this gap is imperative. Business Group on Health’s 2025 Large Employer Health Care Strategy Survey found that MSK conditions continue to be the second-highest cost driver for U.S. employers.
There are multiple reasons why these costs are skyrocketing, but also multiple solutions.
Following my recent webinar with fellow industry experts, Navigating the MSK Epidemic — and new research from the Hinge Health 2024 State of MSK Report — it’s a good time to explore what’s driving MSK costs and outcomes, and how employers can impact both.
What is driving MSK cost and prevalence trends?
From my perspective as a quadruple board-certified physician in internal medicine, pediatric medicine, neonatal-perinatal and bariatric medicine, the scope of the MSK cost problem is broad:
- Employer healthcare costs are rising, especially for MSK conditions. In a recent WTW survey, employers projected a 7.7% increase in their 2025 healthcare costs, up from 6.9% this year. Annual per-member MSK spending specifically has increased by an average of 8% from 2021-2022, compared to pre-pandemic levels in 2019. This makes it extremely difficult for employers to manage their healthcare budgets.
- 1 in 2 Americans experience MSK-related pain. If half of the overall population is affected, it’s likely that half of employees are too. MSK conditions range from back pain and tendonitis to arthritis and osteoporosis.
- MSK prevalence is fueled by an aging workforce. Older employees — who have stayed in the workforce for a variety of reasons — are already at risk for more serious MSK conditions such as osteoarthritis, degenerative disc disease and joint issues.
There are also other factors impacting employer MSK costs.
What is deepening the MSK cost epidemic?
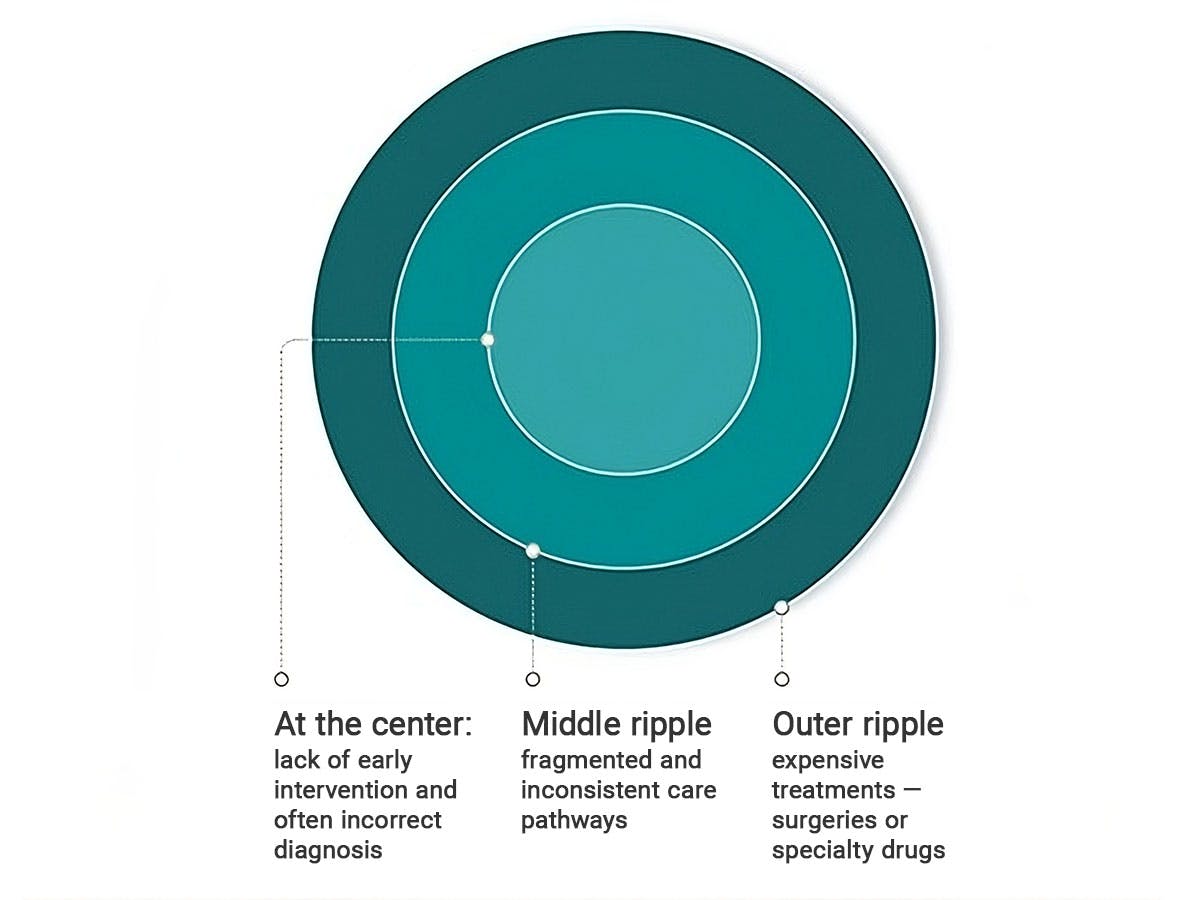
Healthcare costs rise for multiple reasons, and often from care that is not patient-centered. The Cost Ripple Effect explains multiple trends related to MSK’s financial impact on employers:
- The outer ripple is created by expensive treatments such as surgery or specialty drugs.
- The middle ripple arises because care pathways for MSK treatment can be fragmented and inconsistent.
- The core of these ripples is lack of early engagement.
One thing is common across these ripples, employees who:
- Do not understand their pain. Research shows that 60% of people with MSK pain feel that they don’t have control over their condition. Another 48% do nothing and simply “deal with it.”
- Do not understand their benefits. To further complicate things, 46% of health plan members do not fully understand their MSK benefits, which directly affects their ability to manage and treat their conditions effectively.
- Do not receive the right care at the right time. Across the board, members aren’t being guided to the right care. This leads to avoidable injuries and costs.
Collectively, these factors delay appropriate treatment, exacerbating conditions and leading to higher costs.
What are MSK’s preventable paradoxes?
Adding to the problem, many MSK cost and care challenges are counter-intuitive:
- Members want to avoid more expensive treatments but are more likely to receive them. Even though 77% of health plan members say they prefer non-surgical options, their treatment often includes surgery or specialty drugs due to delayed care and provider preferences.
- These expensive treatments are both overused and often ineffective. Why? Because they are treating the wrong or incomplete causes of MSK pain, which rarely exist in isolation. For example, 44% of people who experienced pain in the past 12 months have also experienced anxiety.
- Meanwhile, the best treatments are underutilized. Physical therapy (PT) is the best first-line treatment for chronic MSK pain, but fewer than 10% of all American adults use PT in a given year.
PT is just one part of a conservative yet holistic care plan for MSK conditions that is essential for achieving better outcomes.
What strategies can employers activate to improve MSK costs, outcomes and satisfaction?
Here, it’s important to return to the MSK Cost Ripple Effect. The bad news is the lack of early engagement at its core. The good news is that there are multiple ways that employers can guide their members to the right care at the right time.
From my seat, here are the five most effective strategies employers can use to manage MSK conditions across the workforce and to evolve their benefits strategy.
- Provide proactive prevention, education and engagement. Employers must empower employees to effectively manage their MSK conditions. The emphasis should be on non-invasive treatments and digital care solutions.
- Deliver value-based care via centers of excellence (COEs). Value-based care (VBC) is a healthcare delivery model that rewards providers for the quality, not quantity, of care they deliver and their patient outcomes. COEs include top-performing providers who are held accountable for delivering high-quality care. A RAND Corporation analysis of Carrum Health results data shows that the VBC-COE combination is effective. The approach has reduced unnecessary procedures by 30% and saved employers 45% per episode of care.
- Increase access through hybrid care solutions. In the case of MSK, hybrid care combines in-person therapy — in the provider’s office or at home — with digital care. This involves meeting members where they are and making it easy for them to find and access high-quality, value-based care.
- Address social drivers of health (SDoH). It is now well-known that 80% of health outcomes are based on non-clinical factors like a person’s financial, food and housing security — even their access to reliable transportation. To meet SDoH needs, clinicians and employers alike must lead with empathy, build trust and provide personalized, ongoing support.
- Create a seamless member experience. Multiple specialists are often involved in MSK treatment. That makes it critical to have a single provider manage and coordinate both in-person and digital care. It should be easy for members to navigate the care they need.
Providing a seamless member experience applies not only to MSK treatment but also MSK health benefits. A solution like Quantum Health’s comprehensive navigation and care coordination platform provides a single point of access that guides employees to the right support across all available benefits.
Using our unique model and MSK point solutions, Quantum Health engages with more than 80% of member households representing 85% of medical claims costs incurred. The result for employers is a healthier, more productive workforce with lower per-member costs and a health benefits budget that is more predictable and affordable.
I firmly believe that collaboration is key.
Partners working together — while creating a seamless member experience that’s easy to navigate — is the best way to help members get the right MSK care at the right time, which benefits everyone involved.
