COVID-19 is accelerating disruptive changes in how, where and when consumers see their primary care providers. Employers and navigation have roles to play in maintaining this key connection.
Sometimes described as healthcare’s “quarterbacks,” primary care providers (PCPs) play a critical role in helping self-insured employers control claims costs and achieve positive outcomes.
Research shows that consumers who begin healthcare journeys with a PCP (often a family, general or internal medicine doctor) incur costs at a rate 33% lower than those who go directly to a specialist. Routinely seeing a PCP has been shown to reduce the odds of premature death by nearly 20%.
Because the consumer-PCP connection is so pivotal, Quantum Health works intensively to get more of our clients’ benefits plan members choosing and seeing a PCP. In year one, on average, we’re able to boost by more than 5% the number of plan members who designate a PCP.
Cracks in the consumer-PCP connection
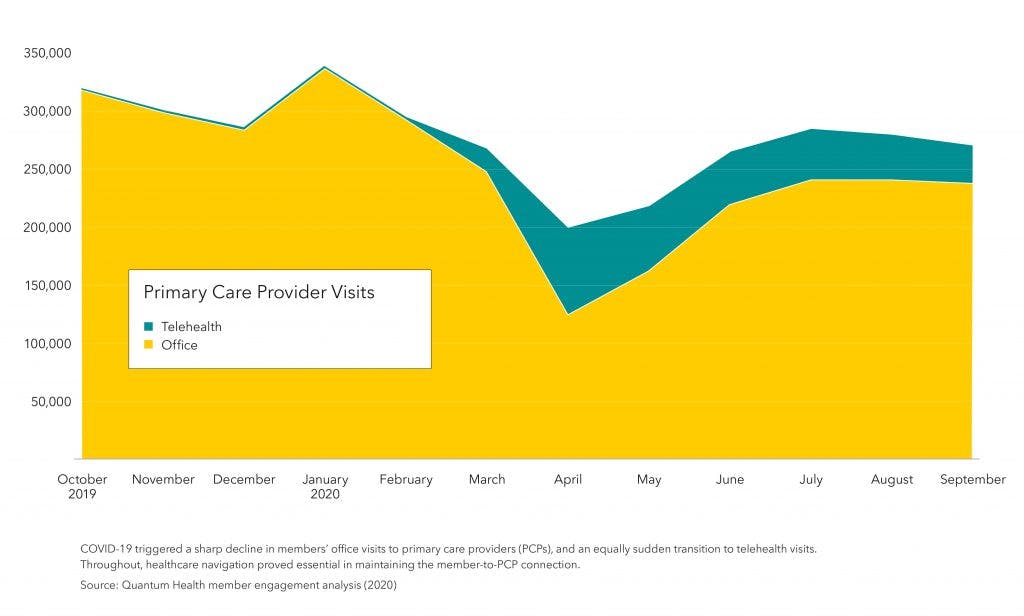
COVID-19 brought historic disruption to primary care. The accompanying chart shows the plunge in PCP office visits by plan members during the pandemic’s initial surge. Doctor’s offices, clinics and hospital systems nationwide saw similar drops in patient visits.
In analyzing the causes, we expected to find members expressing concerns about coronavirus exposure or incurring copay and claims costs. But their primary barrier to PCP visits? Lack of access.
Doctor’s offices were struggling to adapt to COVID-19’s impacts. As they became short staffed, some had to reduce hours and discourage symptomatic patients from coming in for routine care. Further contributing to the squeeze: More than 16,000 physicians’ offices closed during 2020.
During the year’s second half, in-person PCP visits trended higher but remained well below historic norms. At the same time, as the chart shows, PCP appointments via telehealth spiked. This overnight evolution in primary care has important implications for benefits professionals.
Insights from the front line
Many industry analysts predict that the traditional primary care pathway has changed fundamentally and will continue evolving.
What some describe as “a decade’s worth of virtual care transition” during 2020 will likely cause use of telehealth, remote monitoring and other virtual health services to stay elevated. Employers are expected to seek more virtual options from provider networks and point solution partners. With this will come the challenge of gaining enough utilization to ensure cost savings and member convenience goals are met.
Meanwhile, research shows employers exploring other strategies to support primary care access. These include establishing on-site or near-to-campus clinics, as well as contracting with vendors that offer comprehensive primary care service models.
As the format and location of primary care shifts, the COVID-19 experience reveals why navigation is key to sustaining the consumer-PCP connection.
For example, employers, consultants and providers have hustled to include or expand virtual care in their plans and practices during 2020. Throughout, Quantum Health’s navigation has kept providers continually updated on benefits eligibility and timing, plus guided members through rapidly shifting care options.
During the pandemic surge (and anytime members struggle to reach a PCP for immediate needs), our member services and clinical Care Coordinators have served as a primary care “bridge.” Examples include guiding members to urgent care instead of the emergency room when appropriate, answering treatment plan questions, and pursuing prescription refills when members lack time to make what might be repeated calls to their PCPs.
Aside from how and where they eventually “see” a PCP, consumers often won’t do so on their own without persistent education and prompting. For employers, it’s essential that someone engages with your members routinely, pinpointing those who lack a PCP and guiding them to make that cost-saving, risk-mitigating connection.
