As more employees struggle with behavioral health, benefits leaders need a clear understanding of their needs to provide effective solutions. For U.S. workers and employers, 2020 appears to have been a behavioral health inflection point.
- A mid-year survey by Lyra and the National Alliance of Healthcare Purchaser Coalitions found 83% of employees experiencing emotions associated with poor mental health, and 40% believing their employers don’t care, beyond how it might affect their productivity.
- A 2019 Mercer survey showed that more than half of employers and nearly 70% of large employers consider behavioral health a serious concern. Still, only 30% feel they’re being effective with outreach to employees who struggle with mental health and substance use.
As employers and benefits consultants pursue strategies to narrow this gap, Quantum Health continually monitors trends in our member interactions, seeking useful insights. Specifically, we’ve analyzed:
- How, during the latter half of 2020, behavioral health issues presented in conversations between our front-line Personal Care Guide (PCG) nurses and members.
- What benefits guidance or clinical support we provided in response to members’ concerns.
The many facets of employee mental health
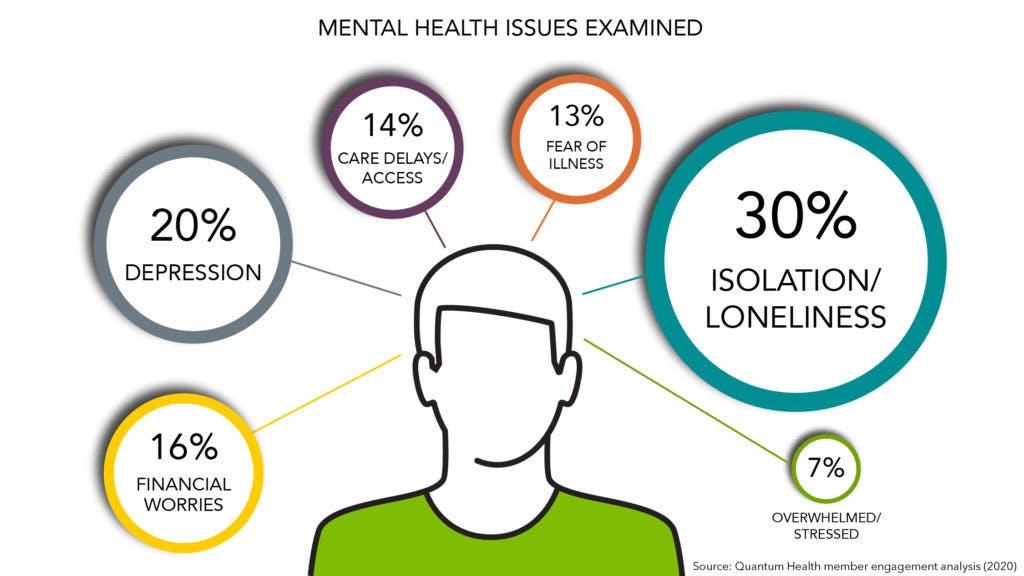
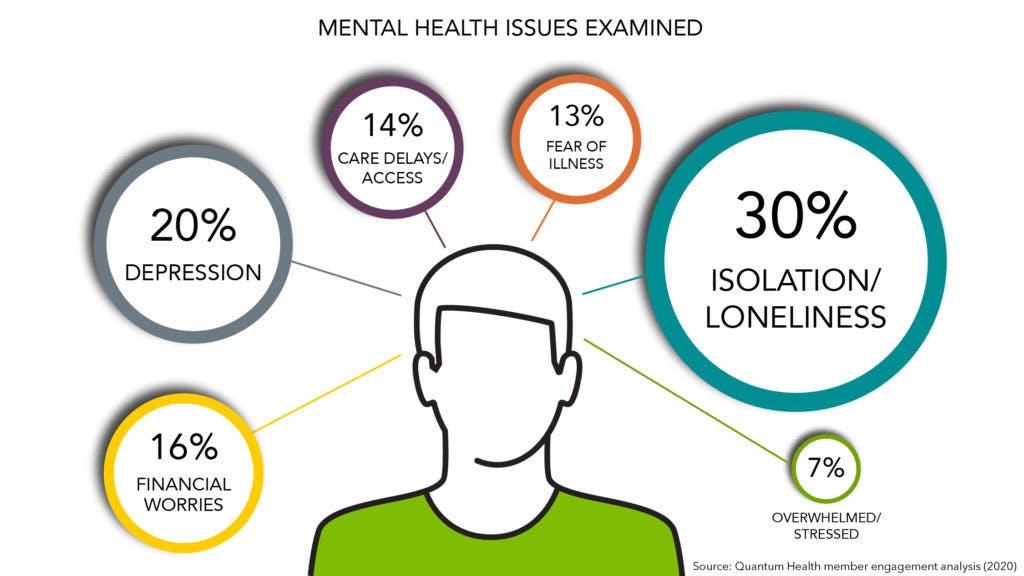
Distilling thousands of member engagements, the analysis revealed:
- In most engagements, members’ issues ranged from generalized feelings of depression, stress and anxiety to financial worries, loneliness and isolation, or fear of contracting an illness (the latter two usually in a COVID-19 context).
undefinedundefinedundefined
Insights from the front line
Employers have reason to be concerned about identifying and supporting employees with major depression, anxiety and other disorders. PHQ-2 screening is one critical way Quantum Health supports that priority.
However, our engagement analysis suggests most workforce mental health challenges take other forms. It also indicates that most employers already offer meaningful mental health support, benefits employees aren’t always aware of, especially in stressful moments when they need the benefits most. Driving awareness and utilization of those benefits takes empathetic, active-listening engagement.
That’s where healthcare navigation and care coordination can play essential roles in your mental health strategy. For example:
- When a member contacts Quantum Health about eligibility or claims related to a family member’s serious medical diagnosis, our Care Coordinators not only provide answers, but also frequently ask a conversation-starting question, such as: “How is everyone doing?”
- Because they are in ongoing care coordination with members, PCG nurses often become trusted sounding boards for members inclined to share feelings. For more reticent members, PCGs are in position to proactively inquire about and assess well-being on an ongoing basis.
As one PCG noted: “There are diagnosable mental illnesses, and then there are people struggling with stresses in life. To get at these issues, it’s critical that we’re in the flow of their overall care. It takes having conversations, so members can share not just their physical pains, but also their emotional ones.”
Relevant, actionable health benefits insights
Subscribe to Navigation Insider
Subscribe