In this insightful video from the EBN Benefits at Work Conference, Veronica Knuth, chief people officer at Quantum Health, and Leslie Pilliod, vice president of benefits and wellbeing at Target, share their strategy for evaluating new benefits solutions.
Leslie explains that any point solution considered by Target must integrate seamlessly with Quantum Health, which serves as the front door to their benefits ecosystem. This requirement ensures a consistent, streamlined experience for team members. Integration is non-negotiable because it supports their core philosophy: keeping the team member at the center of every decision.
The conversation also touches on the importance of understanding and acting on team member sentiment. Target places a high value on employee feedback, using surveys to assess the effectiveness of their benefits offerings. If something isn’t working, they don’t hesitate to find a better solution that will deliver a positive outcome for their employees and their families.
Watch the full discussion to learn how Quantum Health and Target prioritize seamless integration, consistent experience and employee voice to continually enhance team member wellbeing.
More like this

Empowering MAG employees with personalized healthcare support
With Quantum Health, MAG employees get compassionate, expert support when navigating their care.
Learn more
A seamless healthcare experience for MAG employees
Quantum Health helps MAG employees stay focused on their mission by removing the stress of managing healthcare.
Learn more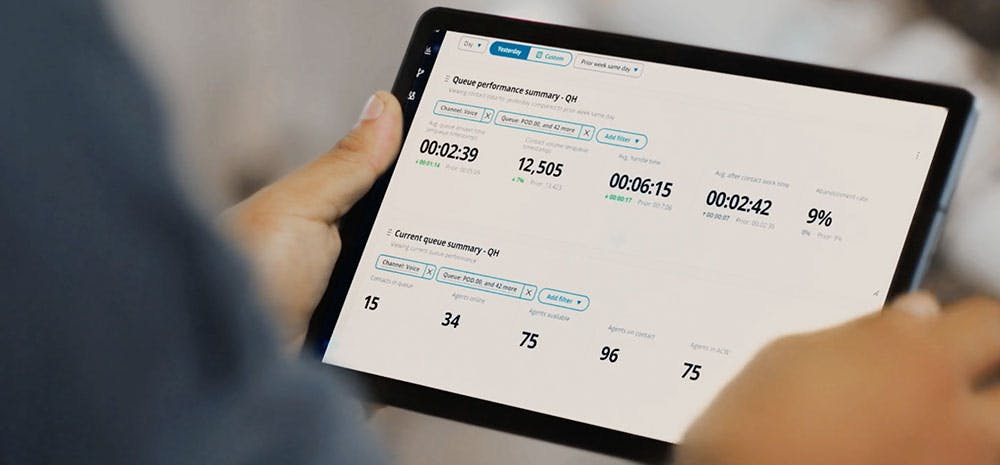
The future of connected healthcare
Experience faster, smarter healthcare navigation. Discover how Quantum Health’s AWS-powered platform delivers seamless, connected care.
Learn more