Social determinants of health (SDOH) defy simple benefits solutions. But a non-traditional member engagement strategy, informing focused plan changes, can combine to make a meaningful difference.
As benefits professionals strive to help employees and their families stay healthy, while also controlling claims costs, social determinants of health (SDOH) stand as a significant and stubborn barrier.
The World Health Organization defines SDOH as “the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life.” The Kaiser Family Foundation (KFF) groups these nonclinical health factors into six broad categories:
- Economic stability
- Neighborhood and physical environment
- Education
- Food
- Community and social context
- Healthcare system (insurance coverage and benefits literacy, for example)
All these factors can have a negative impact on health. Researchers at the University of Wisconsin’s Population Health Institute created a model for measuring and ranking U.S. counties on health outcomes and contributing factors. Their model attributes as much as 50% of outcomes to a combination of clinical care and lifestyle behaviors. The remaining 50% are attributable to SDOH, including a person’s physical environment, plus a range of social and economic factors, from income and education level to family and community support.
With SDOH playing such a major role in health outcomes, HR teams and benefits advisors face the persistent challenge of how to solve for them in member populations. Navigation Insider recently explored the subject of SDOH with Quantum Health’s clinical team. The takeaways can be useful as you explore ways to tackle these powerful, but often elusive, factors affecting your members’ health.
Insights from the front line
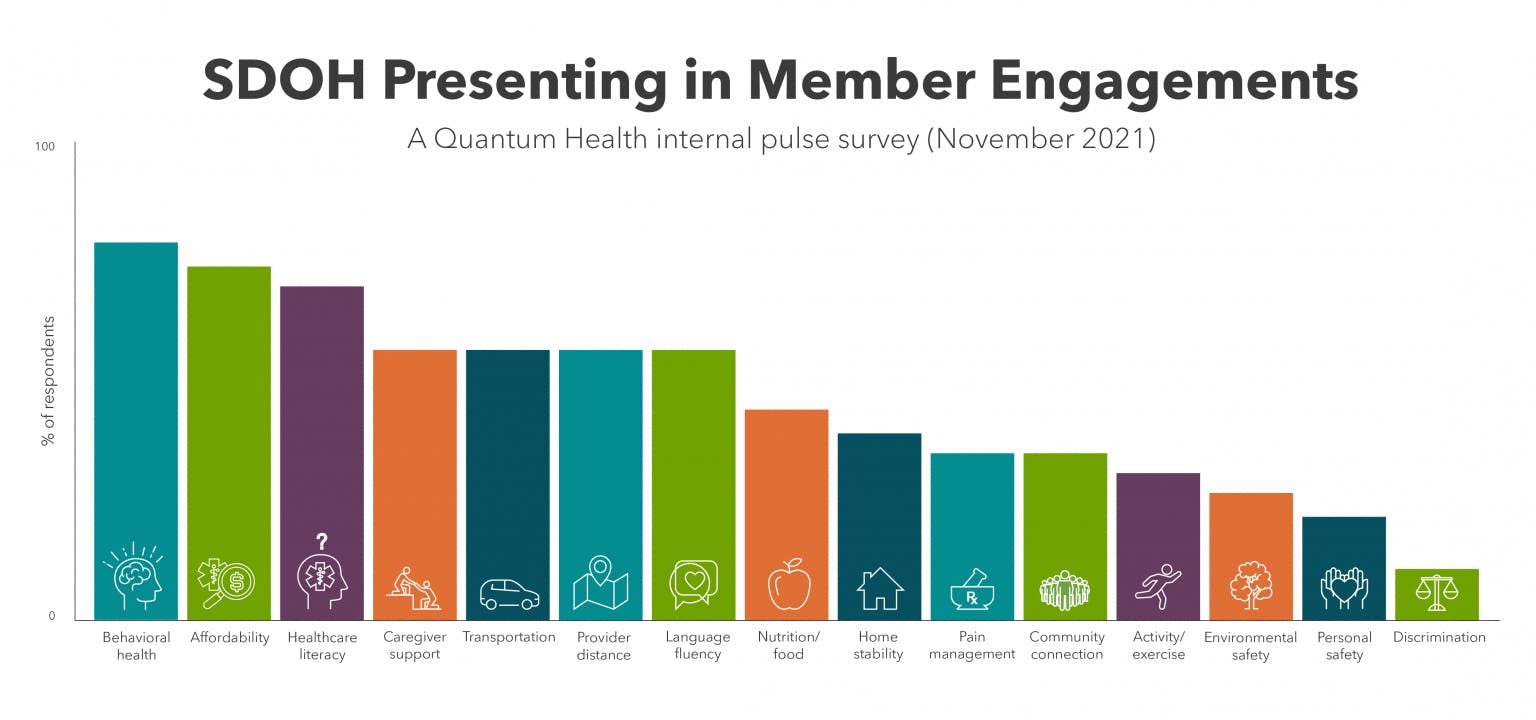
We surveyed our clinical team leaders to gauge which specific SDOH might be present in Quantum Health’s thousands of daily engagements among more than 2 million members.
Our survey broke KFF’s categories into 15 more-specific SDOH challenges. The findings reveal that today’s members face the gamut of SDOH issues. All 15 challenges have surfaced in member engagements during the past 12 months. The four we encounter most often are:
- Healthcare and benefits literacy
- Behavioral health disorders
- Concerns over ability to afford medical care and prescriptions
- Difficulty accessing providers because of distance or lack of availability
Dr. Michael C. Sokol, Quantum Health’s senior vice president, clinical strategy, said he empathizes with HR leaders and benefits advisors, because SDOH pose multiple obstacles to traditional benefits solutions. Since SDOH are so varied, there’s no all-purpose point solution. SDOH also aren’t limited to a demographic or socioeconomic cohort — literally anyone can find themselves facing a barrier to physical or emotional health. When they do, it’s often not something they’re eager to share with HR colleagues, or even with a primary care provider.
To make progress on addressing SDOH, Sokol said, employers can consider taking steps to expand benefits coverage, especially in areas of your plan where a focused enhancement could make a difference. Using our pulse survey as an example, that might mean increasing the number of mental health counseling sessions covered by an EAP. Or it can involve working with network and telehealth partners to ensure members facing access barriers have virtual care options. Employers would want to conduct original research to learn which SDOH are most common or urgent among their own members.
Why the member engagement model matters
Beyond considering plan changes, Sokol said, a self-insured employer’s member services model and engagement strategy play a pivotal role in spotting and solving members’ specific SDOH issues.
Using Quantum Health’s core healthcare navigation and care coordination services as an example, he said, members with SDOH challenges receive wide-ranging support from our Care Coordinators, including our Personal Care Guide nurses. The nurses’ clinical expertise and empathetic benefits guidance combine to build trusting relationships, making some members more comfortable disclosing barriers to their well-being. Often that means our nurses can start problem-solving an SDOH issue during the same chat session or call when it first surfaces. Examples include:
- Early recognition of intervention opportunities. During even the most basic member inquiry (such as replacing a lost benefits ID card), our Care Coordinators are trained to probe a member’s health status and any near-term benefits or health concerns. The goal: Detect upcoming care for which that member needs help understanding benefits; provide guidance to high-quality, cost-effective providers; and attempt to solve any SDOH barriers.We are also the single point of contact for providers to confirm benefits eligibility and coverage. That means providers’ requests for service authorizations signal us to engage with members early in cases that could become physically, emotionally and financially complex.
- Preadmission and postdischarge calls. SDOH can be especially harmful when they hamper a member’s recovery from a hospital stay. Factors that might lead to a poor outcome, even readmission, include insufficient caregiving support, inability to interpret and follow discharge instructions, and lack of transportation to follow-up doctor or therapist appointments.
Quantum Health’s model includes preadmission and postdischarge conversations with a member and, in many cases, their primary caregiver. During both interactions, our nurses seek to uncover and solve SDOH issues before they become roadblocks to a member’s recovery. - Behavioral health assessment. Our PCG nurses conduct a depression assessment on the spot when a member interaction indicates one is appropriate. The Patient Health Questionnaire-2 (PHQ-2) screen gives our nurses immediate insight into whether referral to mental health benefits and specialty care is called for. This integrated approach helps ensure that members get the assistance they need, when they need it, and that employers’ investments in mental health benefits get used as intended.
- Referral to community and educational resources. In addition to their in-depth understanding of an employer’s benefits plan, our nurses have access to a deep and expanding database of community resources and health services. These range from local disease support groups and discounted transportation providers, to financial assistance programs offered by hospitals and drug companies. Combined, it gives our Care Coordinators an ecosystem of possible solutions to SDOH issues, so they can help each member get the support they need.
Problem-solving at a highly personal level
Sokol said Quantum Health’s engagements with members offer frequent reminders of just how nuanced SDOH challenges — and the highly personalized solutions — often become. Here are a few examples:
- It’s not uncommon for our PCG nurses to contact local adult protective services after learning a member is living in an unsafe environment or abusive relationship.
- A member who was struggling to afford funeral services for her deceased husband was anxious to the point of despair and neglecting her own health. One of our nurses immediately stepped in to help. She reached out to several local funeral homes, eventually finding one willing to work with the member.
- When a nurse identified a member needing mental health support, she made a “warm transfer” to the EAP, with the member still on the phone. Because the EAP was not accepting new patients, our nurse contacted the client’s HR team. Together, they quickly devised a plan for the member to see a psychiatrist and have it covered by the EAP benefit.
- A member whose wife was in hospice care with metastatic breast cancer was struggling to afford a power wheelchair for her. Our PCG nurse and Care Coordinators worked closely with the member and a local durable medical equipment supplier, which ultimately provided the chair at no cost.
“These stories always remind me that, for many SDOH scenarios, there just isn’t a conventional, off-the-shelf answer,” Sokol said. “It requires being absolutely committed and creative in coming up with ways to help that member in need. Not all member services models are built, or have the resources, to come up with those types of solutions. And they can ultimately have a huge impact on members’ health and quality of life.”
Given the variety and complexity of SDOH, and the highly individualized scenarios that play out in members’ lives, Sokol said SDOH will continue to pose challenges for employers and their benefits plan. But, he added, there are ways to make consistent, meaningful impact and progress.
Those options include adopting an enhanced member services and engagement model, which helps identify and problem-solve for SDOH on an ongoing, member-by-member basis. SDOH insights gained from those engagements create a powerful data set that employers can use to inform future benefits plan enhancements. Combined, these approaches should yield better health outcomes, despite the complexities posed by SDOH.
