Benefits Experience
6 Insights Employers and Advisors Should Know About the Employee Benefits Experience
SHARE

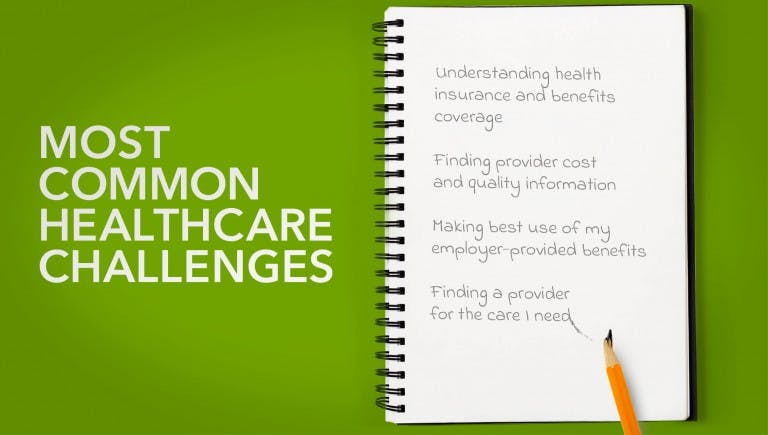
HR teams and consultants work hard to design health benefits strategies that support and satisfy employees and their dependents. But how well do members understand your carefully crafted plans? From finding providers and understanding coverage limits to navigating point solutions and digital apps, do they sail through or struggle when accessing healthcare?
For answers and insights, in March and April Quantum Health surveyed 1,001 consumers who’d experienced healthcare in the past two years. These were adults 18 to 64 who receive benefits through an employer with 1,000 or more employees. To gain employers’ perspective, we also surveyed more than 250 benefits decision-makers at self-insured organizations with 1,000 or more employees.
Below are six research-based insights benefits pros might want to factor into their planning discussions.